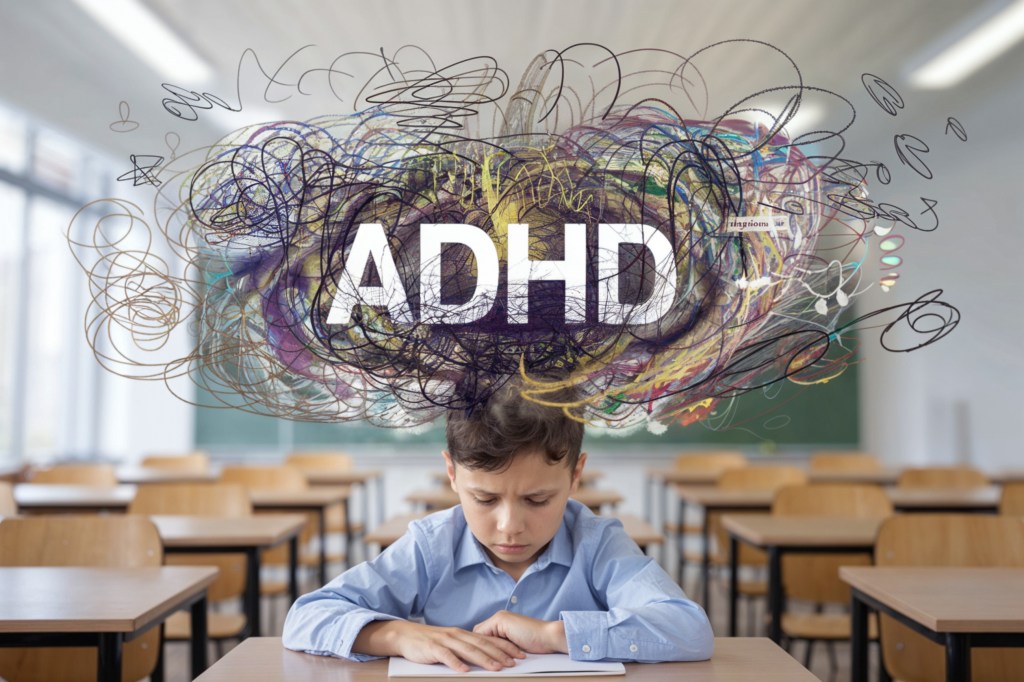
Attention-Deficit/Hyperactivity Disorder (ADHD) is one of the most common neurodevelopmental conditions in children, affecting attention, behavior, and self-control. An estimated 6 million children in the U.S. have been diagnosed with ADHD (Centers for Disease Control and Prevention [CDC], 2023). While parents play a crucial role, schools are equally important in creating an environment where these children can thrive academically and socially.
1. Early Identification and Support
Teachers are often the first to notice signs of ADHD, such as difficulty staying focused, impulsive behavior, or struggles completing assignments. When concerns arise, schools can connect families with appropriate evaluations and resources. Early recognition allows for timely intervention, reducing frustration for both students and teachers (National Institute of Mental Health [NIMH], 2023).
2. Classroom Accommodations
Structured support helps children with ADHD reach their potential. Through 504 Plans or Individualized Education Programs (IEPs), students may receive accommodations like:
- Extended time on tests and assignments
- Preferential seating close to the teacher
- Frequent breaks to manage restlessness
- Simplified, step-by-step instructions
These small changes can make a significant difference in learning and confidence (American Academy of Pediatrics [AAP], 2019).
3. Positive Behavioral Strategies
Children with ADHD often face criticism for disruptive behavior. Instead, schools can promote positive reinforcement by acknowledging effort and progress rather than only pointing out mistakes. Reward systems, consistent routines, and visual cues support behavior management while building self-esteem (CDC, 2023).
4. Teacher Training and Awareness
Educators need the right tools to support diverse learners. Professional development on ADHD can help teachers understand classroom strategies, cultural considerations, and how to collaborate with parents and healthcare providers. Training also reduces stigma, ensuring students feel supported rather than singled out (NIMH, 2023).
5. Collaborative Partnerships
The best outcomes occur when schools, parents, and healthcare providers work as a team. Regular communication ensures consistency in expectations and strategies across home and school. Schools can also connect families with counselors, psychologists, or social workers who provide additional support (AAP, 2019).
6. Promoting Healthy Routines in School
Daily exercise breaks, mindfulness activities, and opportunities for hands-on learning can help students with ADHD stay engaged. Encouraging physical activity and reducing excessive screen time during the school day also support focus and self-regulation (Healthy People 2030, 2020).
The Bottom Line: Children with ADHD can thrive when schools provide structure, compassion, and collaboration. By implementing accommodations, training staff, and partnering with families, schools can empower students to learn with confidence and succeed inside and outside the classroom.
References
American Academy of Pediatrics. (2019). Clinical practice guideline for the diagnosis, evaluation, and treatment of ADHD in children and adolescents. Pediatrics, 144(4), e20192528. https://doi.org/10.1542/peds.2019-2528
Centers for Disease Control and Prevention. (2023). Data and statistics about ADHD. https://www.cdc.gov/ncbddd/adhd/data.html
Healthy People 2030. (2020). Children with ADHD who get treatment. U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. https://health.gov/healthypeople
National Institute of Mental Health. (2023). Attention-Deficit/Hyperactivity Disorder. https://www.nimh.nih.gov/health/topics/attention-deficit-hyperactivity-disorder-adhd